It is so often that we read prescriptions
with "No extension exercises" or "Advised flexion
exercises". Patients advised to prolonged bed rest in
supine position with pillows under the knee, although study after
study has been suggesting the better effects of movement and
exercise and the ill-effects of prolonged bed rest.
Let us look at the study
results of what this famous position offers to the average back
pain patient.
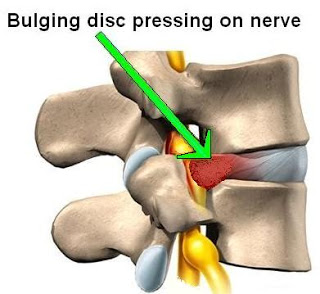
Position of nucleus
in two supine position using MRI in asymptomatics (Beattie
et al 1994). Supine lying with
the hips and knee in flexion has traditionally been advocated as
the appropriate position off rest for individuals with LBP which
was challenged by Cyriax and McKenzie. Distance of posterior margin of NP to posterior
margin adjacent vertebral margin was greater in extended position
introducing a roll under the low back than in supine position with
pillow under the knee, in L3/4, L4/5, and L5/S1. There was no
difference in anterior position. The NP of degenerated did not move
in the same way as normal disc. Williams maintained that LBP is
often caused by lumbar lordosis placing an excessive stress on the
posterior bony and soft tissue structures of the lumbar spine.
According to McKenzie and Cyriax, increased lordosis results in anterior
displacement of the NP with a decrease in the pressure on the pain
sensitive structures in the neural foramen. The above
(Beattie et al 1994)
study proves it all.
Would you still advice your patients to
rest with pillows under knee to induce flexion in the
spine?
As study after study has revealed to us,
that it is difficult to anticipate a stereotypical response within
the disc to changes in position, consistent with clinical theory,
would it not be in the best interest of your patients quick
recovery that exercises be based on symptomatic response to
movement and positions.
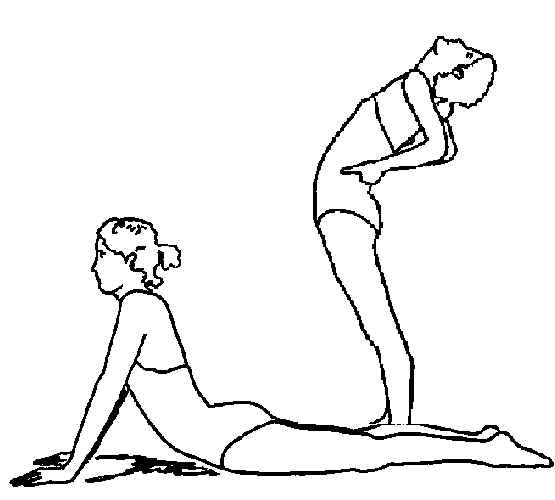
Mechanical Diagnosis and Therapy (MDT) or
famously called 'The McKenzie Concept" is a low technology
assessment system which is well researched.
Managment using McKenzie concept follows the
diagnostic classification, based on symptomatic and
mechanical response to movement, positions and postures.
MDT is evidenced to be reliable between
clinicians who are trained in it, to bring out responders and
non-responders. In responders we would know how best to help your
patient control their pain and prevent their recurrences, and when
and how they would need our help to control their pain
in the least number of sessions. We do not need any
expensive investigations, nor gadgets to recognise non-responders
to the system. Our structured assessement and clinical
reasoning is all that
is
needed.
RCT
Reliability Studies in MDT
or (McKenzie Concept) -
Prognostic Studies in MDT
(McKenzie
Concept)-
RCT
(McKenzie
Concept)-
Cost effectiveness
(McKenzie Concept)-
.
Can the herniated
discs be reduced?
Study on porcine cervical spine. Evidence of reversal of
prolapse with specific movement, position. (Scannel & McGill,
2009). Looked at effects of flexion, extension and lateral flexion.
Concluded that the herniated disc could be reduced with reversal
testing.